Interdisciplinary Rounds Improve Patient Care
The Three Cs to Success
The Woodland Hills Intensive Care Unit has built a speak up culture with interdisciplinary rounds on patients. As a result, the team has high morale, low turnover—and its patients suffer fewer hospital-acquired infections.
Consistency, collaboration and communication pay off for Woodland Hills ICU team
Elizabeth Rollice, RN, always knew that the Intensive Care Unit at the Woodland Hills Medical Center in Southern California was a great place to work.
As a staff nurse there, she and her co-workers enjoy good teamwork and excellent communication, and they deliver high-quality care to the sickest patients.
Now they have proof of their success.
This spring, the unit received the Gold Beacon Award for Excellence from the American Association of Critical-Care Nurses, the world’s largest specialty nursing organization. The award recognizes hospital units that demonstrate exceptional care through improved outcomes and greater overall patient satisfaction.
The team will be honored at the National Teaching Institute & Critical Care Exposition in San Diego, May 18-21.
“I knew that we did a good job and that everyone worked well together,” says Rollice, a member of UNAC/UHCP and a representative on the department’s unit-based team. “This award validates the quality of our work and tells us, ‘Yes, we are doing a pretty good job.’ ”
What’s best for the patient
Superb communication and a culture of collaboration among all members of the care team are key to the team’s success, enabling the consistent practice of evidenced-based medicine that has improved the quality of care.
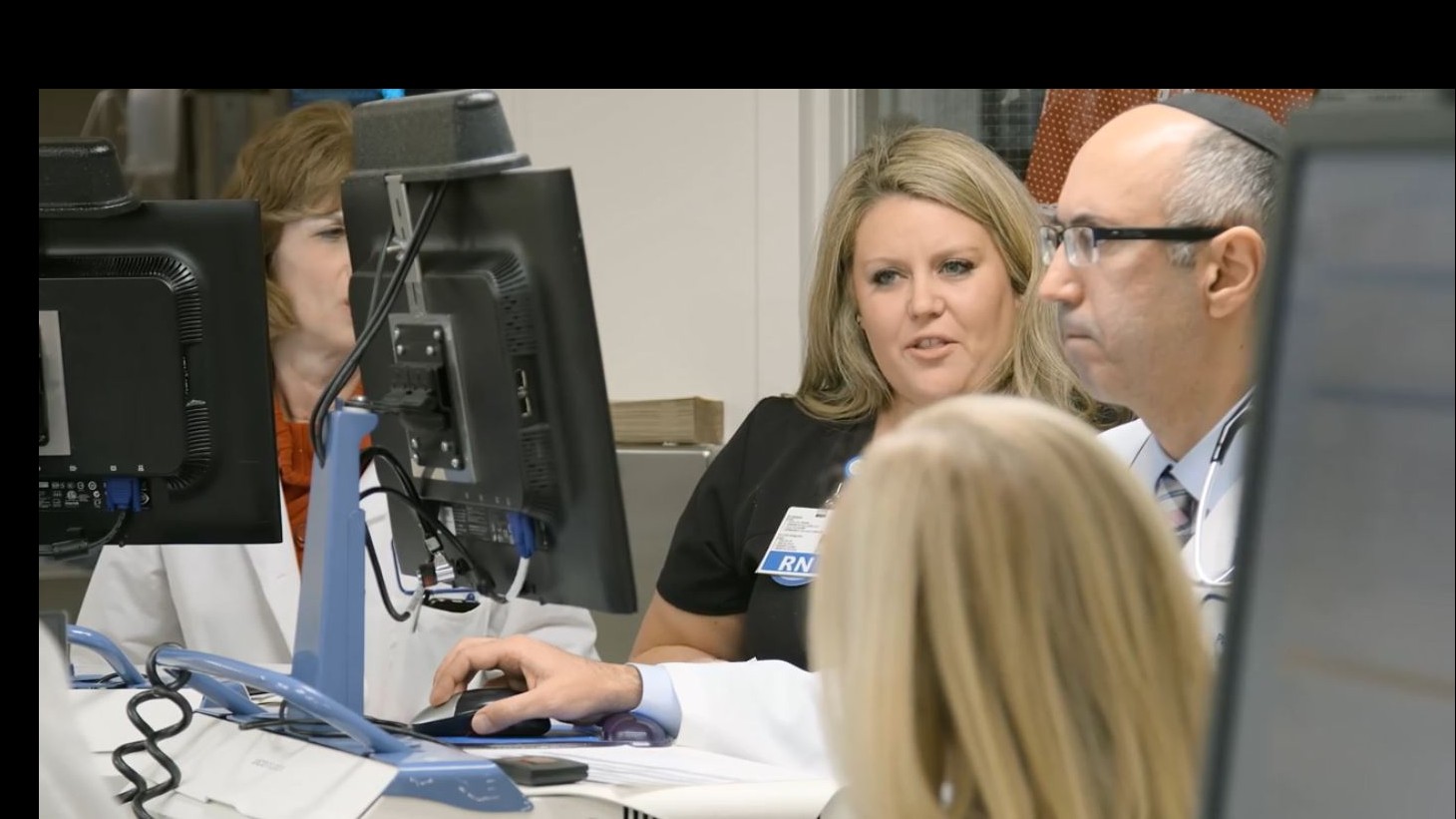
Daily multidisciplinary rounds, for example, involve everyone on the care team who touches the patient.
“It’s about working in partnership with physicians, nurses and other staff to deliver high-quality care based on the newest evidence,” said Lynne Scott, RN, a clinical nurse specialist for the Critical Care and the Definitive Observation Unit. “We’re constantly moving forward.”
Nurses say team rounding gives them an opportunity to speak up and influence care decisions that affect their patients.
“We’re able to talk together about what’s best for the patient,” said Erica Bruce, RN, a UNAC/UHCP member who is the team's union co-lead. “If I feel that something is inappropriate, then I get a chance to ask the doctor. Family members get to ask questions about their concerns, too.”
Multidisciplinary rounding has produced an unintended benefit—higher member satisfaction. “I started in the ICU in 2002. We didn’t have a big rounding team at the time. Families sometimes felt unsupported,” recalls Paramjeet Dhanoa, RN, a staff nurse and UNAC/UHCP member. “Now that we have a big team, our families are more satisfied, because they feel they are not alone in making decisions. They are more comfortable.”
Open communication
Communication is vital in a department where staff members work around the clock in rotating shifts. To ensure information is consistently shared from shift to shift, the team:
- practices Nurse Knowledge Exchange Plus (NKE Plus)
- holds monthly UBT meetings, with members of the representative team responsible for sharing information with individual staff members
- holds quarterly staff meetings; those who miss the meeting must review the staff meeting binder and sign a form indicating they’ve read it
- uses a bulletin board to post important news and activities
The bulletin board, sandwiched between the nurses’ station and the staff restroom, attracts passersby with colorful fliers and posters.
“Your eyes are drawn to that communication board,” Rollice says. “You pass by a wall full of fliers, notes and postings, you can’t help but stop and look. It’s in a prime location.”
Conducted at the patient’s bedside, NKE Plus provides nurses with a template for patient safety and communication.
“It helps promote open communication and it helps us understand what’s going on with the patient,” says Judy Stone, RN, a staff nurse and UNAC/UHCP member, of the structured, in-depth, face-to-face handoff between the outgoing and the incoming nurse.
Stone says an additional itemized checklist “forces us, as nurses, to have all the pieces of the puzzle ready in the morning for multidisciplinary rounding. It really focuses us on everything that is going on with the patient so that we can deliver the best care that we possibly can.”
Clinical successes
Building the culture of collaboration and openness has had a big payoff:
- No ICU patient has contracted VAP since the first quarter of 2011.
- There have been no central line-associated bloodstream infections since the fourth quarter of 2011.
- The unit achieved the 86th percentile on the HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) patient satisfaction survey from January 2013 through August 2014.
“To consistently deliver the best patient outcomes, you must have the processes and structures in place,” says Kareem Younes, RN, nursing project coordinator for Woodland Hills. “It’s about doing the right thing at the right time, every time.”
Going for the gold
While earning the Beacon Award was hard work, completing the 50-page application was perhaps even tougher for the Woodland Hills ICU team.
Few on the six-member representative UBT had writing experience, and they were at a loss when it came to telling their story in a way that would satisfy the award committee.
That’s when the team turned to in-house consultants Scott and Younes. Even with their expert help, the team faced data collection challenges and grappled with complex questions about the quality of their clinical practice.
At times they failed to meet, making it difficult to complete the application. And at one point, members were forced to make a “course correction” and rewrite the application when the guidelines changed unexpectedly.
“The rewrites were really painful,” recalls Sharon Kent, RN, the department’s administrator and UBT management co-lead. “It was like writing a thesis.”
Despite the challenges, team members said the process was rewarding because it enabled them to see their work in a different light.
“It made us take a closer look at the work we do,” says Rollice. “It motivated us to do better. It made us want to achieve the gold-level standard of care.”
